Genetic Testing for Dental Disease Risk
Pamela Woolford BSc (Hons) MSc Nutritional Medicine R. Nutr. RDH, Health Promotion Certificate (Open)
When the Human Genome Project which successfully mapped all 25,000 genes that comprise humans was completed, it sparked an avalanche in our understanding and knowledge of the powerful relationship between our genes and the environment.
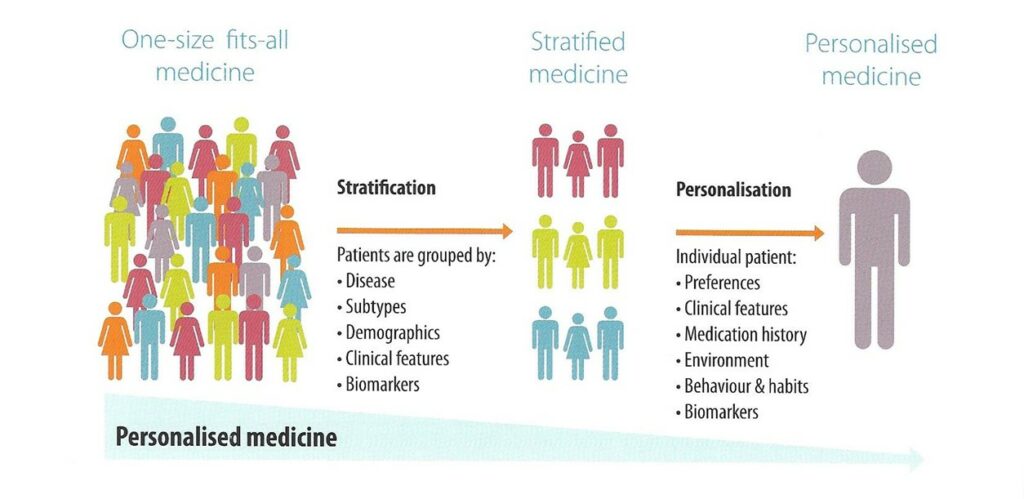
This relationship is now becoming more mainstream and Personalized Medicine is now emerging as a new strategy in prevention, diagnosis and treatment of disease.
By knowing an individual’s unique genetic makeup, lifestyle and nutritional interventions can be targeted specifically to that individual’s needs.
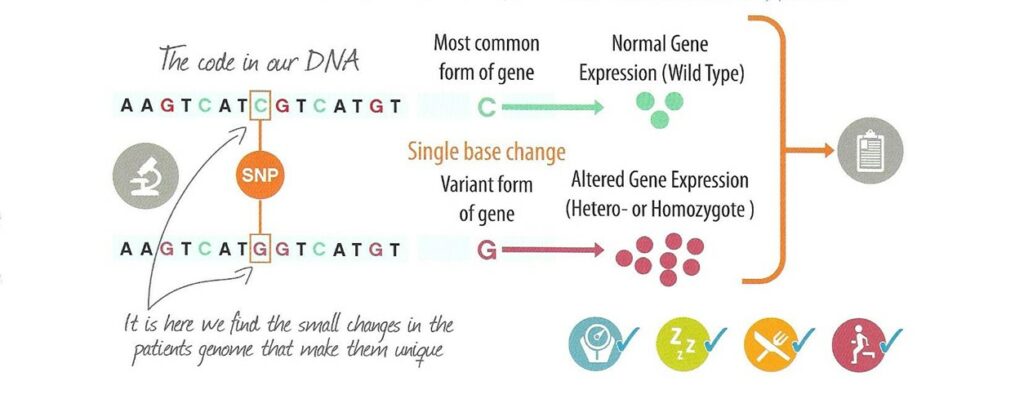
Genes are made up of DNA (deoxyribonucleic acid) from which proteins are made. We have two copies of each gene inherited from our parents.
Human DNA consists of over 3 billion nucleotide base pairs, of which more than 99% are identical in each one of us.
The 1% consists of small variations know as Single Nucleotide Polymorphisms (SNPs), these have a variation in a single nucleotide that occurs at a specific position on the DNA. One lone SNP does not usually cause disease, but can give a susceptibility to a disease especially under environmental exposures
Genetic testing looks for these SNPs which can have a strong influence on the functioning of the gene in which it is found. This can alter biological pathways within the cell in which that gene functions and affect metabolic processes that are important for health.
Having the knowledge of this gene variant means that certain dietary and lifestyle interventions can compensate for the effect this gene variant would have.
To analyse the DNA a blood spot test is taken and sent off to a laboratory offering these tests.
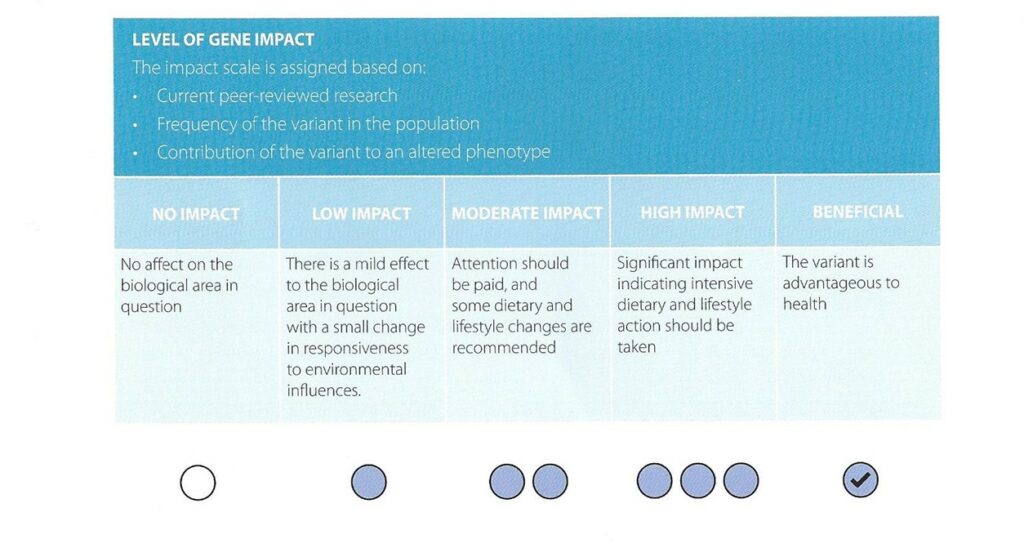
The test result is presented in a report which gives a list of all the genes that have been requested to be analysed. This report describes the impact the SNP variant would have on certain metabolic and biochemical pathways
Some gene variants are advantageous while others may contribute of an increased health risk.
The level of impact is indicated in the test report by an impact scale.
GENETIC TESTING FOR SUSCETIBILITY TO DENTAL DISEASES
Results of a genetic test carried out on a patient to assess the risk of periodontal disease and susceptibility to caries.
Apart from dental health Periodontal Disease has also been linked to an increase risk for other chronic inflammatory diseases such as Coronary Heart disease (1), Type 2 Diabetes (2), Obesity (3) and Alzheimer’s disease (4).
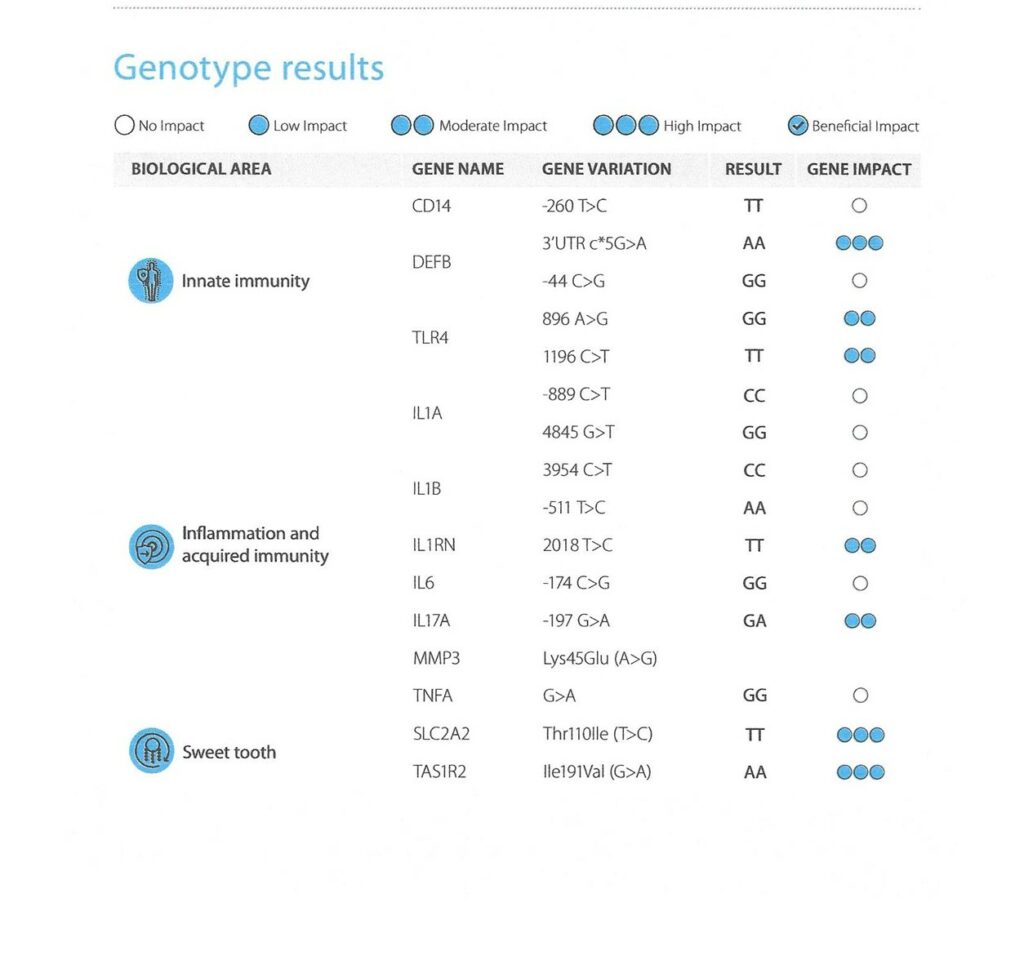
As you can see from the table below, three biological areas are looked at:
Innate Immunity
Inflammation and Acquired Immunity
Sweet Tooth
Innate Immunity
Comprises of the physical defensive barriers such as the skin, the general immune response comprising of immune cells and proteins and also includes defensive mechanisms such as saliva. The innate immune system is activated by the presence of antigens and their chemical properties which is dependent upon pattern recognition receptors (PRR) which detect pathogen – associated molecular patterns (PAMPs) which are structures on pathogens such as bacteria, virus, bacteria and protozoa.
As you can see from the Genotype Results Panel, this patient does have an altered innate response when exposed to endotoxins and pathogenic bacteria contributing a moderate increased risk for developing Periodontal Disease and Type 2 Diabetes
The DEFB gene variation codes for the beta-definsin 1 protein. This is a antimicrobial peptide implicated in the resistance of epithelial surfaces to microbial colonisation
The TLR4 gene variation is important in the inflammatory process and contributes to susceptibility for periodontitis. TLR4 cytokine expression is significantly increased in both macrophages and gingival fibroblasts located in inflamed gingiva.
Inflammation and Acquired immunity
Acquired immunity also called the adaptive immunity develops over a lifetime as you are exposed to infections, disease or vaccinations. Inflammation and the inflammatory response are important factors to consider with acquired immunity. Cytokines are produced and are associated with chronic low grade inflammation which contributes to an exaggerated response in infections.
As you can see from the Genotype Results panel, 2 genes are affected and this gives a moderate increased risk for chronic low grade inflammation and related inflammatory disorders. This is due to increased expression of pro inflammatory cytokines and an altered response to endotoxin and bacterial exposure.
The IL1RN gene variation leads to a more active inflammatory response as an important leverage point in the inflammatory cascade and is also a regulator of the extracellular matrix where increased expression leads to osteoclastic degradation.
The IL17A gene variation encodes for a proinflammatory cytokine Interleukin -17A and is a strong contributing factor in the pathogenesis of various autoimmune and inflammatory diseases. Increased levels have been found in the saliva of patients with periodontal disease.
Sweet tooth
Genetics contributes to the individual variability in sugar consumption, where sweet taste receptors and glucose sensors contribute to an individual’s sweet craving behaviour and sugar intake and so a risk for caries.
As you can see from the Genotype Results Panel this patient has a risk of having a sweet tooth.
The SLC2A2 gene variation codes for the GLUT protein which acts as a glucose sensor and is implicated in post prandial satiety if this is reduced as in this genotype it is associated with consumption of higher amounts of sugar than usual.
TheTAS1Rs gene variation encodes the taste receptors which are strongly involved in sensing sweet taste in foods. This genotype is associated with altered receptor function leading to higher sugar intake and seeking out sweet tasting foods.
Clinical Implications of using this test
Oral hygiene excellence was the first implementation that was given to this patient but also by using this test, lifestyle, nutrition and targeted dietary supplements were recommended to the patient to help negate the genetic risk that was revealed. The patient became more aware of not only the risk to oral health but also to systemic health which the patient was not aware of before.
With the use of these genetic results the patient could see their genetic risk for periodontal disease and dental caries. This becomes a very strong behavioural change motivator, with this information this patient became more focused on their oral hygiene routine and was more motivated to adopt a healthier dietary intake.
Correspondence pam@yourabundantlife.co.uk
REFERENCES:
- Periodontal Disease, Systemic Inflammation and the risk of Cardiovascular Disease Carrizales – Sepulveda EF et al Heart, Lung and Circulation 2018 Nov 27 (11) 1327-1334
- (Periodontitis and Diabetes; a two way relationship. Preshaw P Diabetolgia 2012
- Association between Obesity and periodontal Disease. A systemic review of epidemiological studies and controlled Clinical Trials. M. Martinez-Herrera et al Med Oral Patol Oral Cir Bucal , 2017 Nov1;22(6);e708-715
- The Role of Periodontitis and Periodontal Bacteria in the Onset and Progression of Alzheimer’s disease; A Systematic Review. Dioguardi M, Crinocoli V et al Journal of Clinical Medicine 2020 Feb 11;9(2);495.

